So, what is the point in this post? I suppose the main question I would like to explore is: Whether/ how cannabis should be used medically in our society (the UK specifically)? I am going to approach this from a medical perspective, because although there are other remits which one could explore, I am not hugely determined to pursue these branching avenues on the past uses, political aspects or the recreational uses. I would like to try and highlight the mechanisms of action that cannabis has, and how this may and has been used therapeutically.

As one of the most abused drugs in the world, and there seems to be an ever-growing inconsistency between the science behind cannabis and the myths. I feel there is a split between these pseudo-scientists who seem to think cannabis will be some sort of panacea for all earthly ailments and those who are so anti that they remain obstinate in the face of actual evidence.
The former claiming some senseless benefits such as ‘lighting up unlocks your creative potential and helps you lose weight’, whilst also failing to mention the myriad of downsides such as risk of psychosis, cardiovascular disease, infertility and general mental health problems. The latter giving either contradictory or irrelevant information (such as cannabis increases the risk of car accidents, I mean, so does a blindfold, just not sure how it is a downside just don’t drive).
At the end of the day there is probably valid points from both sides of this 10,000-year-old fence. And it undoubtedly comes down to type and moderation. I mean the risk to someone who makes their own hempseed milk and is “partial to some whacky-tobacco” is negligible in comparison to someone who smokes skunk daily.
Definitions
I think it would be useful to first separate some terms so that there can be no confusion. During the course of this blog Cannabis will be used to denote both Hemp and Marijuana, technically both of these substances are classed as cannabis, but their morphology, and chemical make-up are very different. Cannabis belongs to the family (Cannabaceae) that has just one genus (Cannabis), there are several species of cannabis from sativa to indica to ruderalis, the largest variety being cannabis sativa. It is a dioecious plant which means it can be separated into male and female plants, each with different properties[1]. Hemp is a variety of Cannabis sativa L and has a variety of uses from the fibre in the stems to make ropes (some hemp ropes have dated back to 26,900 BCE)[2], fabrics, paper and building materials. The seeds can be used as fuel or food and the leaves and flowers can be cultivated into CBD oil [3] Marijuana comes from the Indian Hemp seed and is cultivated purely for the intoxicating effects of its female flowers/buds. [4]
Tetrahydrocannabinol (THC) and Cannabidiol (CBD)
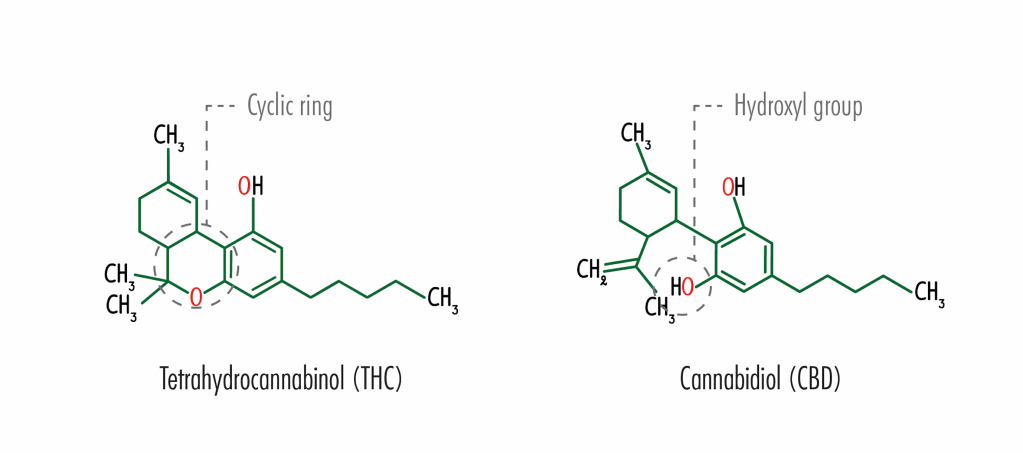
So where exactly does the intoxicating and therapeutic effect of these cannabis plants come from? These plants produce a huge array of phytochemicals (biologically active compounds in plants) including a broad range of cannabinoids, famously including tetrahydrocannabinol (THC) and cannabidiol (CBD). The notorious yin and yang of cannabis. There are actually over 60 different types of (Phyto)cannabinoids within cannabis with THC and CBD just being two of them [5]. These cannabinoids work in our body on something called the Endocannabinoid system (EC). The EC system is a molecular system that is responsible for regulating numerous processes within the body, these include the immune response, cellular communication, appetite, memory and many others. For something that has such a crucial role in the body, it is surprising to note that the EC system wasn’t discovered until ~ 30 years ago by a molecular biologist named Lisa Matsuda [6]. Before delving into the workings of the EC system it would be worth mentioning some knowledge of basic neurotransmission may be useful. (If you understand Action potentials, synapses and neurotransmitters then you can skip this bit then read on, if not here is a link to another blog that will explain it: (https://neuro7.home.blog/2020/06/04/the-basics-of-neurotransmission/)
The Endocannabinoid (EC) system
The EC system relies on 3 essential components: The endocannabinoids (the natural cannabinoids made by the body), The receptors (molecules that the endocannabinoids can bind to) and the enzymes (these break down the endocannabinoids once their role is complete). The EC systems communicates messages slightly differently because it does it ‘backwards’, so essentially when the post synaptic neuron is activated by the neurotransmitter it causes the creation of endocannabinoids (they are of Neurotransmitters for the EC system) that can then travel back toward the pre-synaptic neuron where they attach to cannabinoid receptors. This is important because they can act as a sort of dampener, controlling how much neurotransmitter (e.g. dopamine) can be released in future [7].
There are two main types of cannabinoid receptor (CB1 and CB2) that when bound to cause varying effects depending on where there are in the body and what endocannabinoid it is bound to. CB1 receptors are primarily found in the brain and central nervous system, these CB1 receptors seem to mediate many of the psychoactive effects of cannabinoids. The CB2 receptors are distributed throughout the immune system and peripheral nervous system and seem to be responsible for anti-inflammatory and other immune system responses [8]. It’s on the EC system that these Phyto-cannabinoids: THC and CBD play a role.
Mechanisms and therapeutic potential of THC
THC is a molecule that can mimic these endocannabinoids. When someone ingests THC, the body may be overrun with the substance thus interfering with the natural cannabinoid within the body. I have heard the clichéd line “we have marijuana receptors in our body” which isn’t strictly wrong but is rather misused. Instead it should be “we have receptors in our body that marijuana can bind to and mimic the effect of the natural endocannabinoid neurotransmitters”. THC can bind to both CB1 and CB2 very strongly and because these receptors are everywhere the overstimulation by THC causes such a wide variety of effects, some good some bad [9].
They are in the Amygdala which controls emotions such as fear and anxiety and thus overstimulation induces a paranoia effect. They are in the Basal ganglia which is an area of the brain which helps start our movement (over stimulation causes slowed reaction times). They are in the Hippocampus controlling memory formation (and thus forgetfulness) and the Hypothalamus controlling appetite (and thus the munchies). These are just some of the area that these CBs inhabit but we can already see how overstimulation by THC will cause problems all over the body and brain [10][11].

THC is not all doom and gloom and there are potential treatments using THC due to the fact that it can bind to these CB receptors very strongly. It therefore can have many similar effects to the natural cannabinoids and also some of the effects that CBD can cause. It will act as a pain reliever, reducing nausea, anti-inflammatory and increasing appetite so there are definitely benefits to the use of THC. There are indeed approved medical treatments that use just THC such as oral THC (Marinol) that is approved for use in the US to treat nausea and vomiting due to chemotherapy; however, for me, what it comes down to is that everything THC can do, CBD can do it better and with fewer side effects. In fact, the only areas where THC seems to blaze a trail is in its ability to induce a “high” and also increase appetite.
Mechanisms and therapeutic potential of CBD
That’s THC, but what about CBD – this apparent panacea. One of the key differences between the effects of both these substances is that CBD doesn’t have the intoxicating effects that THC has this is because it is not psychotropic and doesn’t strongly bind to these CB receptors mentioned above. There are various ideas as to how CBD actually acts on the body, with some suggesting it works by preventing the breakdown of the (natural) endocannabinoids thus causing them to have a longer lasting effect on the body. Studies have also shown that CBD can also bind to a variety of other receptors such as 5HT (Serotonin Receptors), TRPV, GPR55 and can also change the shape of the CB1 receptor preventing THC from binding directly to it [11].
Regardless of what exactly it binds to, CBD can bind to a lot of receptors, great! But what does this mean therapeutically? after all that’s what this comes down to. Is there a viable purpose other than as a recreational drug, to which a resounding answer would probably be: Yes.
5HT: For instance, by binding to 5HT, CBD may have a useful role in treating many disorders (such as depression and psychosis). This family of serotonin receptors are found throughout the nervous system. Tangentially when studying these topics, I am always astounded by the sheer multitude of effects that a single family of receptor can have in the body. Serotonin is no different and is said to influence various processes such as aggression, anxiety, appetite, cognition, learning, memory, mood, nausea, sleep and many others. I mean leave something for the other receptors. It is therefore purported that CBD can cause some antidepressant effects by binding to this 5HT receptor [12] .
There is also evidence proposing CBD as a treatment for psychosis as research has shown that the EC system itself may be involved in psychosis (with psychosis patients showing a higher level of the endocannabinoid (anandamide) and increased CB1 receptors) It is hoped CBD may effectively act as an act as an atypical antipsychotic, without the undesirable side effects which are often seen from other antipsychotics (what are termed extrapyramidal side effects (EPS))(some examples of other atypical drugs are clozapine and risperidone) [13][14]. The evidence at this point is reasonably sparse, with the need for more high-quality randomised control trials. There has been a couple of good quality trails (such as by McGuire et all in 2018) which have shown CBD to cause a slight improvement of positive symptoms of psychosis (these symptoms such as hallucinations and delusions) while also showing an improvement in the patient’s cognition and the impact of the illness on their day-to day lives. Further studies using patients suffering from psychosis (rather than animals or healthy participants) will allow for a wider array of concrete evidence. Finally, there is also evidence that suggests CBD provides an anti-emetic (anti-sickness) effect by indirect activation of a specific 5HT receptors in an area of the brain called the dorsal raphe nucleus [15]. The activation is therefore useful as a treatment for nausea caused by chemotherapy (in reality in a direct comparison between THC and CBD for treating nausea THC seems to perform better, in this case it may be a combination of both that proves most effective.)
TPRV1: CBD can also binds to this TPRV1 (Transient Receptor Potential Vanilloid Type 1), which is linked to the immune function and inflammation, pain, and control in the hypothalamus [16]. This will lead to some supposed analgesic (pain relief) effects of CBD, more specifically it has been shown to be an effective anti-hyperalgesic (hyperalgesia is an abnormal increased sensitivity to pain) for acute inflammation and chronic pain. Generally it seems CBD has promising effectiveness as an anti-inflammatory agent for nervous tissue inflammation, arthritis, IBD (Inflammatory Bowel Disease) and potentially certain types of cancer that are linked to chronic inflammation[17][18].
Epilepsy: Finally, CBD has some very proven effectiveness on Epilepsy. This is one of the most common serious neurological condition, with about 1 in 100 people having active epilepsy and ~ 1 in 50 people who will develop epilepsy during their life [19].
It is a group of disorders characterised by abnormal electrical activity in the brain, leading to unprovoked seizures. Epilepsy is a disorder which has no single diagnostic test that gives a definitive yes or no. There is not a single drug or treatment that is effective as a cure, the general consensus for drug treatment with epilepsy is to “start low – go slow”, where the goal is to find an effective treatment with the lowest drug treatment or combination that works.
(There are ~25 drugs that can be used to treat epilepsy as a monotherapy, when this doesn’t work as a treatment duo-therapy can be used (two drug therapy) leading to ~ 300 different drug combinations that may be effective. If the duo-therapy is not effective, then 3-drug treatment options can be used with about 2300 different combinations).
Even after all this, the treatment will only be effective in about 70% of cases, not to mention the fact that some of these drug treatments have some pretty dire side effects (such as Valproate, which can cause stomach upset, hair loss, tremor, bruising, and damage to an unborn child). What this really comes down to is that there are still ~30% of epilepsy cases that are untreatable by AEDs (Antiepileptic drugs) [20]. This is where treatment a substance such as CBD may be particularly useful. Dravets syndrome is a serious epilepsy that manifests in the first year of life and often lead to future difficulties such as poor language development, poor motor skills and development of chronic illness. There is also 20% mortality by age 20. It is also an epilepsy that is particularly resistant to AEDs.
This is one of the disorders where the use of CBD has been authorized as a potential treatment. There is evidence to show that CBD can half the the number of monthly seizures. This may be because CBD is able to inhibit receptors in the body (such as FABPs (a fatty acid binding protein) and the GPR55 mentioned earlier) that other AEDs don’t interact with [21][22] thus causing the natural endocannabinoids like anandamide to have a longer lasting effect in the body
Conclusion
Initially returning to the original question of “Whether / how cannabis should be used medically in the UK?” to be blunt: Yes. Obviously not for every known ailment, but there is undoubtedly evidence for cannabis (Either CBD or THC) being a valuable therapeutic tool across a wide range of conditions. The fact that we have a substance that can treat symptoms of nausea, anxiety, depression and appetite, while also being able to improve outcomes on debilitating diseases such as Epilepsy, psychosis and multiple sclerosis must give it some position to be credited as a valuable instrument in a health care professionals (HCPs) tool kit.
I think it partially comes down to is how we view and use these substances. Cannabis was classified as a Class B drug alongside its undoubtedly more dangerous counterparts such as Amphetamines and Ketamine – which can only be administered in a medical setting by trained professionals (and on the occasional horse). Up until 2018 cannabis was classified as having no redeeming value to society and in 2018 the legalisation of medical cannabis seemed like a step in the right direction to embrace its potential. Yet, it seems the British medical establishments remain decidedly unconvinced. A year later it seemed only ~20 NHS prescriptions had been issued (Mostly to infants with lethal epilepsy such as Dravets) [23].
This is probably due to the lack of acceptance from the medical community and also the extremely restrictive criteria laid for patient access. These misconceptions about the whole family of cannabis has created a sort of anti-cannabis hysteria with the only way to change being with real life data. There are of-course good steps being made in this area from numerous published and on-going studies as well as the massive increase in sales of CBD based products in the British retail markets, but there is definitely still a way to go.
Now coming to how it should be used, this poses a slightly more difficult question. For me the answer seems to be in the use of predominantly CBD based products with an aim to have greater regulation over the amount of THC. I don’t think anyone is really expecting a complete legalisation of cannabis both recreationally and medically because in all honesty that’s not beneficial. This country already has an alcohol problem, giving them another recreational drug probably isn’t going to help, possibly the only benefit would be a decrease in the number of street fights outside spoons. What is needed is clearer guidelines for HCPs on the appropriate use of cannabis in the most appropriate form, presumably something like oral CBD, or prescription medication with a low dose of THC. At the end of the day we can always see if Canada has space for us.
Bibliography
1] ‘Hemp uses, information facts – Hemp Basics’. [Online]. Available: https://www.hempbasics.com/shop/general-hemp-information.
[2] ‘Fiber Technology for Fiber-Reinforced Composites – Google Books’. [Online].
[3] ‘Handbook of Cannabis and Related Pathologies: Biology, Pharmacology … – Google Books’. [Online].
[4] ‘What Is Hemp? | The Differences Between Hemp vs. Marijuana’. [Online]. Available: https://weedmaps.com/learn/the-plant/hemp-vs-marijuana/.
[5] Z. Atakan, ‘Cannabis, a complex plant: Different compounds and different effects on individuals’, Therapeutic Advances in Psychopharmacology, vol. 2, no. 6. SAGE Publications, pp. 241–254, 2012.
[6] ‘The Role of the Endocannabinoid System in the Human Body – CURE Pharmaceutical’. [Online]. Available: https://www.curepharmaceutical.com/blog/the-role-of-the-endocannabinoid-system-in-the-human-body/.
[7] P. Pacher, S. Bátkai, and G. Kunos, ‘The endocannabinoid system as an emerging target of pharmacotherapy’, Pharmacological Reviews, vol. 58, no. 3. NIH Public Access, pp. 389–462, 2006.
[8] S. Zou and U. Kumar, ‘Cannabinoid receptors and the endocannabinoid system: Signaling and function in the central nervous system’, International Journal of Molecular Sciences, vol. 19, no. 3. MDPI AG, 13-Mar-2018.
[9] B. E. Alger, ‘Getting high on the endocannabinoid system.’, Cerebrum, vol. 2013, p. 14, Nov. 2013.
[10] ‘The Science of the Endocannabinoid System: How THC Affects the Brain and the Body | Scholastic: Nida’. [Online]. Available: http://headsup.scholastic.com/students/endocannabinoid.
[11] D. A. Kendall and G. A. Yudowski, ‘Cannabinoid receptors in the central nervous system: Their signaling and roles in disease’, Front. Cell. Neurosci., vol. 10, p. 294, Jan. 2017.
[12] E. B. Russo, A. Burnett, B. Hall, and K. K. Parker, ‘Agonistic properties of cannabidiol at 5-HT1a receptors’, Neurochem. Res., vol. 30, no. 8, pp. 1037–1043, Aug. 2005.
[13] J. Renard, C. Norris, W. Rushlow, and S. R. Laviolette, ‘Neuronal and molecular effects of cannabidiol on the mesolimbic dopamine system: Implications for novel schizophrenia treatments’, Neuroscience and Biobehavioral Reviews, vol. 75. Elsevier Ltd, pp. 157–165, 01-Apr-2017.
[14] A. Waldo Zuardi et al., ‘A Critical Review of the Antipsychotic Effects of Cannabidiol: 30 Years of a Translational Investigation’, Curr. Pharm. Des., vol. 18, no. 32, pp. 5131–5140, Sep. 2012.
[15] L. A. Parker, E. M. Rock, and C. L. Limebeer, ‘Regulation of nausea and vomiting by cannabinoids’, Br. J. Pharmacol., vol. 163, no. 7, p. 1411, 2011.
[16] T. Lowin and R. H. Straub, ‘Cannabinoid-based drugs targeting CB1 and TRPV1, the sympathetic nervous system, and arthritis’, Arthritis Research and Therapy, vol. 17, no. 1. BioMed Central Ltd., 06-Sep-2015.
[17] J. M. Nichols and B. L. F. Kaplan, ‘Immune Responses Regulated by Cannabidiol’, Cannabis Cannabinoid Res., vol. 5, no. 1, pp. 12–31, Mar. 2020.
[18] F. Afrin et al., ‘Can hemp help? Low-THC cannabis and non-THC cannabinoids for the treatment of cancer’, Cancers, vol. 12, no. 4. MDPI AG, 01-Apr-2020.
[19] ‘Epilepsy’. [Online]. Available: https://www.who.int/news-room/fact-sheets/detail/epilepsy. [Accessed: 03-Jun-2020].
[20] M. M. Goldenberg, ‘Overview of drugs used for epilepsy and seizures: Etiology, diagnosis, and treatment’, P T, vol. 35, no. 7, pp. 392–415, Jul. 2010.
[21] R. Mechoulam, ‘Cannabis and epilepsy’, Epilepsy and Behavior, vol. 70. Academic Press Inc., pp. 278–279, 01-May-2017.
[22] E. B. Russo, ‘Cannabis and epilepsy: An ancient treatment returns to the fore’, Epilepsy and Behavior, vol. 70. Academic Press Inc., pp. 292–297, 01-May-2017.
